
Departments
Our hospital has a full-time physician who is a certified instructor of the Japanese Society of Spine and Spinal Cord Diseases, and has been actively involved in surgical treatment of spinal cord disorders. Our department primarily performs surgical treatment, and has performed over 2,000 spinal cord surgeries in the last 10 years. For patients who are diagnosed as suitable for conservative treatment (non-surgical treatment such as rehabilitation and medication), we work with local medical departments to refer them to nearby doctors so that they can receive the most appropriate treatment.
An appropriate diagnosis is the most important factor in achieving good surgical outcomes. In addition to imaging findings such as MRI, we also place importance on neurological findings, which can be grasped by carefully examining and touching the patient. Causes can also include brain disease, degenerative diseases of the spinal nerves themselves, and vascular diseases, so we encourage patients to consult with neurosurgeons, neurologists, and cardiologists when necessary, in order to reach an appropriate diagnosis.
Our spinal cord surgery ranges from minimally invasive surgery to comprehensive spinal and pelvic correction and fixation, tailored to each individual's condition. We also actively perform highly challenging surgeries requiring advanced techniques, such as upper cervical spine surgery and spinal tumor resection. Even with the same disease, each patient's condition is far from uniform. Differences in pain, numbness, extent and severity of paralysis, and degree of spinal deformity and degeneration, as well as lifestyle factors such as age, activity level, and occupation, mean that it is crucial to propose and implement the optimal surgical treatment for each individual. Our department strives to always perform safe and reliable surgeries, utilizing cutting-edge surgical equipment, including surgical microscopes, spinal navigation systems, and intraoperative spinal nerve monitoring, as needed. As a result, we achieve favorable surgical outcomes without complications in the majority of cases.
| Cervical spine disease |
|
|---|---|
| Lumbar spine disease | |
| Thoracic spine disease |
|
| General spine |
|
It develops when spinal nerves are compressed due to age-related cervical degeneration (osteophyte formation, disc bulging, ligament thickening, etc.) combined with cervical spine instability and minor trauma. Symptoms often begin with numbness and difficulty moving the fingers (difficulty writing, using chopsticks, buttoning clothes, etc.), and as the condition progresses, symptoms such as tightness in the chest and abdomen, numbness and stiffness in the legs, unsteadiness when walking, and difficulty urinating occur.
It occurs when the intervertebral discs, tissues present between the vertebral bodies of the cervical spine, protrude or slip, putting pressure on the spinal cord or nerve roots. Symptoms often begin with pain and numbness in the neck, shoulders, and arms on either side, and as the condition progresses, symptoms similar to cervical spondylotic myelopathy such as difficulty moving the fingers, numbness and stiffness in the legs, unsteadiness when walking, and difficulty urinating occur.
This condition occurs when the posterior longitudinal ligament, located on the posterior surface of the cervical vertebral body and the anterior surface of the spinal cord, becomes ossified and compresses the spinal cord. It is said to be a genetic factor that is prevalent in Asians, including Japan, but the exact cause is still unknown. The symptoms are similar to those of cervical spondylotic myelopathy. The presence of ossified ligaments on an image does not necessarily mean that symptoms will appear.
This is a condition in which the first cervical vertebra (atlas) is displaced forward relative to the second cervical vertebra (axis). It is often associated with rheumatoid arthritis, but can also develop as a result of trauma. Symptoms include pain centered in the back of the head, but if compression of the spinal cord occurs, it can also cause numbness in the hands and feet and decreased respiratory function.
Although cervical vertebral slippage and instability can occur in people without underlying diseases, they are more likely to occur in people with rheumatoid arthritis, those with a long history of hemodialysis, and patients with athetoid cerebral palsy. The symptoms are similar to those of cervical spondylotic myelopathy, but as cervical vertebral slippage and instability progress, the neck may droop forward, making it difficult to see ahead.
Age-related changes in the lumbar spine (osteophyte formation, disc bulging, ligament thickening, etc.) narrow the spinal canal, which is the nerve passageway, causing compression of the cauda equina and nerve roots. This condition develops when lumbar deformities (osteophyte formation, disc bulging, ligament thickening, etc.) narrow the spinal canal, which is the nerve passageway, and compresses the cauda equina and nerve roots. The condition is characterized by symptoms of intermittent claudication, in which numbness, pain, and tightness from the buttocks to the feet worsen when walking, making it impossible to walk, but the patient is able to walk again after resting in a stooped position for a while. As the condition progresses, symptoms such as muscle weakness in the legs, sensory paralysis, and difficulty urinating appear. Obliterative arteriosclerosis also causes similar symptoms, making it an important differential diagnosis.
Degenerative spondylolisthesis is a disease that develops when age-related changes cause instability in the lumbar discs and facet joints. Slippage occurs between the vertebral bodies, resulting in spinal canal stenosis. It is more common in women over the age of 50, and symptoms are similar to lumbar spinal stenosis, but are characterized by both lower back pain and leg pain.
Lumbar spondylolysis is a disease in which bone loss occurs in the area of the lumbar vertebrae known as the interarticular space, and is said to be caused mostly by stress fractures caused by sports during adolescence. The main symptom is lower back pain when moving, but as with age, if slippage occurs between the vertebrae, pain and numbness in the legs may also occur, similar to lumbar spinal stenosis.
This condition occurs when degeneration of the lumbar disc causes the disc to protrude or slip, putting pressure on the cauda equina and nerve roots. It is most common in people in their late teens to 30s, and symptoms begin with pain from the buttocks to the legs on either side. As the condition progresses, symptoms such as muscle weakness in the legs, numbness, and difficulty urinating appear.
Adult spinal deformity refers to a condition in which the alignment of the spine becomes distorted due to age-related changes such as intervertebral disc degeneration and osteoporosis. Forward curvature of the spine is called kyphosis, and sideways curvature is called scoliosis. When these deformities become severe, not only does it cause lower back pain, but the center of gravity tilts forward or to the side, causing poor trunk balance and making it difficult to stand or walk for long periods of time. People with Parkinson's disease are prone to kyphosis and scoliosis deformities of the spine. Progression of lumbar kyphosis deformity can lead to gastrointestinal symptoms such as gastroesophageal reflux disease, which can lead to poor eating habits.
Lumbar compression fractures are a condition that is often associated with osteoporosis and have been increasing in recent years. For the majority of people, conservative treatment such as wearing a corset and taking medication will allow the bones to heal within a few weeks, and the back pain will be alleviated. However, if the fracture does not heal (a false joint), it can become very stiff and cause back pain, and abnormal movement of the vertebrae can compress the nerves, causing symptoms such as pain and numbness in the legs.
These are tumors that develop near the spinal cord or cauda equina. Benign tumors such as schwannomas and meningiomas are common, but as the tumor grows larger, it can compress the spinal cord or cauda equina, causing symptoms such as leg pain and numbness, leg muscle weakness, sensory paralysis, and difficulty urinating. Schwannomas, the most common type, are characterized by lower back pain and leg pain that worsens at night while sleeping rather than during the day when active. They may be discovered by chance on an image, but once the above symptoms appear, conservative treatment is ineffective and surgical treatment is considered.
This surgery relieves pressure on the spinal nerves by drilling the vertebral body, intervertebral disc, and ligament from the front of the cervical spine for conditions such as cervical spondylotic myelopathy, cervical disc herniation, and ossification of the posterior longitudinal ligament of the cervical spine. It is performed under a surgical microscope to ensure safe and reliable nerve decompression. Bone from the ilium is usually transplanted into the shaved area to reconstruct the spine, and the spine is firmly fixed with a special metal plate to allow for early ambulation after surgery.
This is a surgery performed from the back of the cervical spine to treat conditions such as cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament of the cervical spine. A groove is created in the bone (vertebral arch) that covers the spinal cord from behind in an arch-like shape, and the surgery is opened like a double door to the left and right, relieving pressure on the spinal cord. In our department, we use suture anchors (small fixation devices with threads) developed at Kyoto University to perform the surgery, which allows for shorter surgery times than conventional methods.
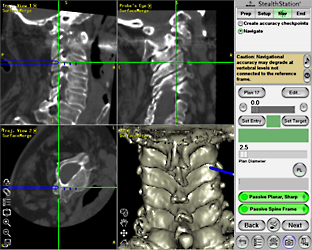
For diseases that require relatively long-range cervical spine fixation, such as those with high instability of the cervical spine due to slippage or correction of kyphosis deformity, we mainly choose posterior fixation surgery. In our department, we use cervical pedicle screws as the first choice, as they are expected to provide the strongest fixation. When placing the screws, we useSpinal Navigation SystemThis combination allows for safe and reliable surgery.

Targeted diseases include atlantoaxial subluxation and atlantoaxial arthropathy, which causes persistent occipital pain. Furthermore, odontoid fractures caused by falls in elderly people have been increasing recently, and we aim to use this method for surgical treatment whenever possible to help patients get out of bed early and prevent them from becoming bedridden. Surgery is performed from the rear of the upper cervical vertebrae, and screws are used to fixate the atlas and axis. Using a targeting device (screw placement device) developed at Kyoto University, we strive to place screws safely and accurately and reduce bleeding.
This procedure is performed for lumbar spinal stenosis with relatively little degeneration of the intervertebral discs or facet joints and no lumbar instability. This is the most popular technique in spinal surgery, and various methods have been reported, but in our department we mainly perform it using the vertical spinous process splitting method. A major advantage of this surgery is that it minimizes damage to the muscles that support the lower back, resulting in less postoperative lower back pain.
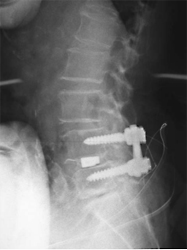
This surgery is indicated for spondylolisthesis accompanied by instability (degenerative spondylolisthesis, spondylolisthesis), foraminal stenosis, and recurrent disc herniation.Fixation of the lumbar spine using metal implantsThis surgery, combined with the use of sufficient bone grafts between the vertebral bodies, provides excellent long-term postoperative stability. This is the most commonly performed spinal surgery at our hospital, and the postoperative clinical outcomes are very good. Single-level fusion allows patients to return to light recreational sports.
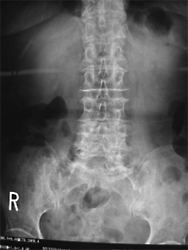
Preoperative

Post-surgery

Conservative treatment is the rule for lumbar disc herniation, but surgical treatment may be considered if selective nerve root blocks are not effective and pain or paralysis makes daily activities difficult. Surgery is usually performed through a 3-4cm skin incision from the posterior lumbar spine, but if certain conditions are met, microscopic MD technique, which can be performed in less than 2cm, is possible. The MD technique leaves a very small surgical incision (the incision is exactly the same size as endoscopic surgery) and is minimally invasive to the muscles, resulting in less postoperative pain, allowing for earlier discharge from the hospital and a faster return to society.
Our department also actively performs corrective fusion surgery for spinal deformities in adults. Depending on the degree of deformity, we may fusion a long area from the thoracic spine to the pelvis. However, by adopting the lateral approach lumbar interbody fusion (OLIF) method using a retroperitoneal approach, which was introduced in Japan in 2013, bleeding during surgery has been significantly reduced, making it possible to perform surgery with less invasiveness than before. In elderly patients or those with complications, this surgery may be performed in two sessions (with an interval of about one week) to reduce the physical burden of the surgery.
This procedure is performed on nonunion joints that occur after osteoporotic vertebral compression fractures. In our department, we perform vertebroplasty using a mixture of autologous bone harvested from the ilium and artificial bone, transplanting a sufficient amount of this material into the nonunion joint, and then using a metal implant. The surgical results are very good in terms of pain relief and expansion of activities of daily living, but continued drug treatment for osteoporosis is essential after surgery.
Our department also actively performs surgery for spinal cord tumors and cauda equina tumors. We strive to perform safe and reliable surgery by making full use of surgical microscopes, intraoperative transdural ultrasound, and spinal nerve monitoring. Over the past 10 years, patients who have undergone surgery in our department and been diagnosed with schwannoma or meningioma have not had to undergo reoperation due to tumor recurrence, and surgical outcomes have been very good. Furthermore, our department treats extramedullary tumors, and refers intramedullary tumors to the neurosurgery department.
For thoracic spinal disorders such as ossification of the posterior longitudinal ligament, thoracic disc herniation, and ossification of the ligamentum flavum, conservative treatment is often ineffective once spinal cord symptoms appear, and surgical treatment is considered. Our department primarily performs posterior decompression and fusion surgery, but depending on the preoperative condition, we may also perform anterior decompression and fusion surgery via a thoracotomy or extrapleural approach. The spinal cord at the thoracic spine is more fragile than other areas, and even intraoperative manipulation or slight changes in position can cause severe paralysis of the lower limbs. As a general rule, we use spinal nerve monitoring to constantly monitor the condition of the spinal cord electrophysiologically, while paying particular attention to nerve safety during surgery.
Total 198 items