
Departments
We treat a wide range of diseases, including degenerative diseases of the cervical and lumbar spine (herniated discs, spinal stenosis, and spondylolisthesis), as well as spinal tumors and vascular lesions.
We are particularly focused on minimally invasive spine surgery. Representative examples include cervical laminoplasty, which enlarges the entire spinal canal through a small incision of approximately 3-4 cm; anterior cervical fusion, which uses the clavicle as a bone graft; transvertebral discectomy, which removes herniated discs through a small hole approximately 6 mm in diameter drilled into the vertebral body; and lumbar intervertebral fusion using CBT, which preserves muscles and nerves. Anterior fusion using the clavicle does not involve any manipulation of the ilium in the pelvis, resulting in no postoperative pelvic pain or numbness, making it a surgical procedure with extremely low complications (this procedure was published in the Journal of the American College of Neurological Surgeons). Furthermore, transvertebral discectomy is indicated for cases in which nerve roots are damaged by lateral cervical disc herniation, preserving most of the intact disc. Both procedures can be performed through a neck incision of approximately 2 cm, offering significant cosmetic benefits.
Cervical laminoplasty can enlarge the spinal canal from the second to seventh cervical vertebrae, making it possible to enlarge the entire spinal canal even in those with a congenital narrow spinal canal or multi-level deformity. The surgery is performed through a 3-4cm skin incision at the back of the neck, and no cervical collar is required after surgery. This allows for early return to work and early rehabilitation.
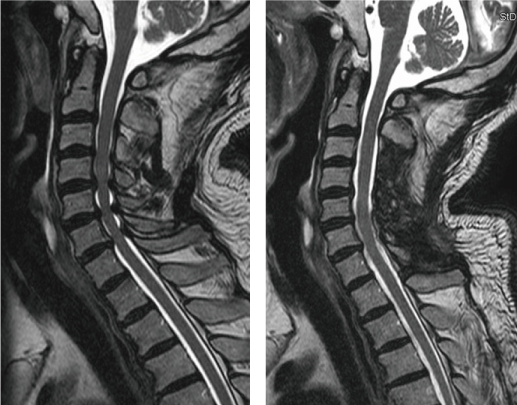
Pre- and post-operative MRI images (the spinal canal has expanded overall, releasing pressure on the spinal cord. In order to protect the soft spinal cord, it is important that the cerebrospinal fluid surrounding the spinal cord is fully filled, using the same principle as a tofu pack.)


CT scan before and the day after surgery
Because bone grafting is performed on the hinge side (right arrow), bone union is achieved early. The patient is able to walk without a cervical collar from the day after surgery. Because the neck can be moved early, it is possible to prevent the reduced range of motion (reduced neck movement) that is a problem with cervical laminoplasty.
Usually, bone grafts are taken from the ilium in the pelvis, but it is also possible to take bone grafts from the collarbone. This surgical procedure has very few complications and does not cause postoperative pain or numbness in the pelvis that makes it difficult to walk (this method was published in the Journal of the American College of Neurological Surgeons).
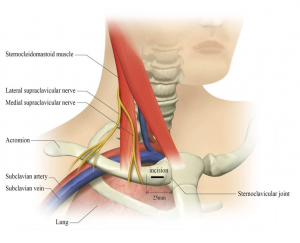
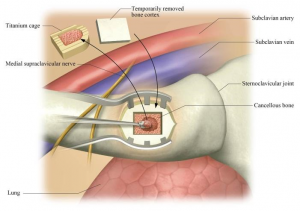
The surgical technique was published in the Journal of Neurosurgery, Spine
A keyhole of about 6-7 mm is drilled into the spine, and only the lesion is removed, preserving the normal intervertebral disc.
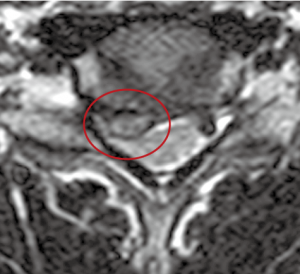
Preoperative MRI image (disk herniation compressing the nerve root on the right side of the midline is observed)
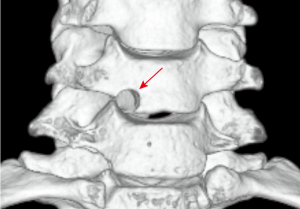
The surgery was performed through a 6-7mm keyhole created in the spine (the arrow indicates the round keyhole).
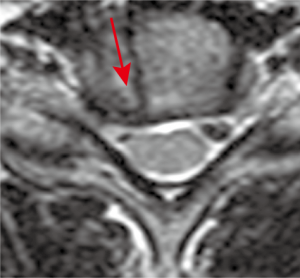
Postoperative MRI image (The herniated disc was completely removed while preserving the intervertebral disc. The arrow indicates the surgical route.)

The 3cm scar on the neck is barely noticeable.
Lumbar spinal stenosis causes intermittent claudication, a condition in which the legs gradually lose movement while walking. Lumbar laminectomy, a surgical procedure to widen the spinal canal, can potentially improve symptoms. However, in cases of lumbar degenerative spondylosis or spondylolisthesis in which the nerve pathways are narrow, lumbar intervertebral fusion, which dislocates and stabilizes the joint, is required. Our hospital performs minimally invasive lumbar intervertebral fusion (MISt), using percutaneous screws to minimize muscle detachment and reduce the risk of chronic lower back pain after surgery. Furthermore, when using CBT (Coritical Bone Trajectory) screws, a method of fixation from the inside to the outside, is available, muscle damage can be minimized, minimizing lower back pain immediately after surgery.
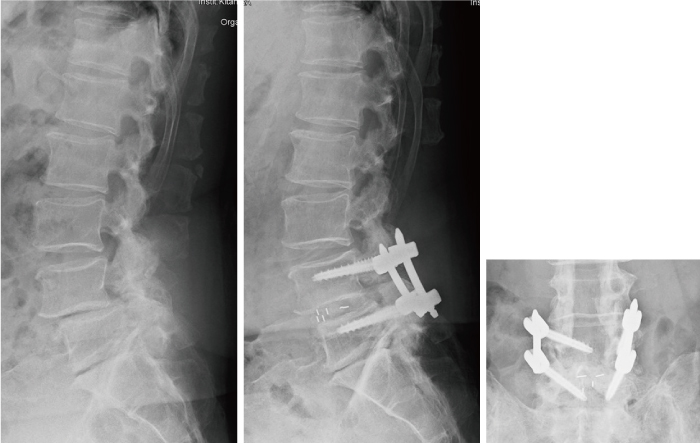
MISt lumbar spondylolisthesis. Center: The preoperative slippage has been corrected. Right: In the frontal view, the screw is facing from the outside to the inside.
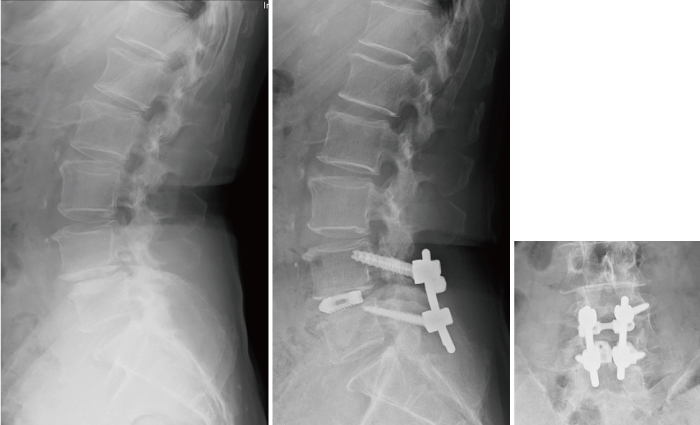
Lumbar intervertebral fusion surgery using CBT. Center: The preoperative slippage has been corrected. Right: In the frontal view, the screws are pointing from inside to outside and from bottom to top.
Are you suffering from numbness in your hands, loss of strength in your fingers, or difficulty walking?
Many patients visit the outpatient neurosurgery department at Kitano Hospital with these symptoms, worried that they may be suffering from a stroke such as cerebral infarction or intracerebral hemorrhage.In fact, these motor and sensory disorders in the limbs are often caused by cervical spinal disorders such as cervical spinal stenosis, cervical spondylosis, ossification of the posterior longitudinal ligament, and herniated discs.
If you are diagnosed with a herniated disc or cervical spinal stenosis, you may be wondering whether you should undergo surgery.
As a basic policy of our department, we do not recommend surgery for incidentally discovered lesions or for mild symptoms of cervical spinal canal stenosis. However, since the condition may worsen following an injury such as a fall, please visit a hospital if symptoms in the limbs appear after an injury. It is recommended that you continue to have regular checkups and imaging tests every six months or one year.
For patients whose daily lives are being affected by cervical spondylosis, surgery may be recommended depending on the severity of the symptoms and test results.
The cervical vertebrae are primarily responsible for supporting the head and protecting the spinal cord within. However, when the bones, ligaments, and discs that protect the spinal cord become deformed, they can compress the spinal cord and nerve roots, which is the opposite of their intended purpose.

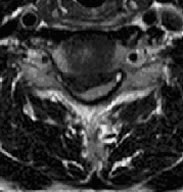
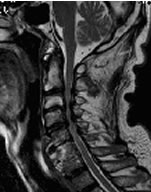
The MRI on the left shows that the disc between the fifth and sixth cervical vertebrae is compressing the spinal cord.
The right horizontal section shows severe compression of the spinal cord and nerve roots.

Broadly speaking, there are two types of surgery: anterior surgery and posterior surgery. Anterior surgery is suitable for removing cervical disc herniations, etc. Posterior surgery is suitable for surgery on multi-level lesions. The choice of surgery is decided based on a comprehensive assessment of symptoms, imaging findings, etc.
In both anterior and posterior surgery, patients are generally allowed to begin walking training the day after surgery. If necessary, a cervical collar will be worn.
Patients are asked to visit the outpatient clinic one month, three months, and six months after surgery, and then every six months to one year for a medical examination and X-rays, CT scans, and MRI scans. Patients are also asked to fill out a questionnaire to understand their condition before and after surgery.