
Departments
| Esophageal Cancer Unit (starting in 2021) Cases studied |
Surgical cases: All cases Minimally invasive surgery using thoracoscopes and laparoscopes (Thoracoscopic laparoscopic subtotal esophagectomy) |
|
|---|---|---|
| 2023 | 19 cases | 4 examples |
| 2022 | 15 cases | 8 cases |
| 2021 | 17 cases | 4 examples |
Esophageal cancer is a unique organ that exists in the mediastinum (chest) and is the only digestive tract, so multidisciplinary treatment that combines not only surgery but also endoscopic treatment, chemotherapy, and radiation therapy is important.
At our hospital, all esophageal cancer patients are examined by our Esophageal Cancer Unit, which consists of specialists in the Departments of Gastroenterology, Medical Oncology, Radiation Therapy, and Gastrointestinal Surgery, and we propose an appropriate combination of treatments. Esophageal cancer surgery is a highly invasive procedure that involves three areas: thoracic, abdominal, and cervical manipulation. However, in principle, all patients are performed using minimally invasive surgery using a thoracoscope or laparoscope. Depending on the location and progression of the esophageal cancer, we also actively perform intrathoracic anastomosis using only a thoracoscope or laparoscope, omitting cervical manipulation, and have reported favorable results.
If you are diagnosed with esophageal cancer, please contact us.
| 2023 | 30 cases (distal gastrectomy: 21 cases, cardinal gastrectomy: 5 cases, total gastrectomy: 4 cases) Of these, 16 were laparoscopic surgeries, 12 were robotic surgeries, and 2 were open surgeries. |
|---|---|
| 2022 | 21 cases (distal gastrectomy: 17 cases, cardinal gastrectomy: 3 cases, total gastrectomy: 1 case) Of these, laparoscopic surgery: 13 cases, robotic surgery: 8 cases, open surgery: 0 cases |
| 2021 | 33 cases (distal gastrectomy: 28 cases, cardinal gastrectomy: 0 cases, total gastrectomy: 5 cases) Of these, 19 were laparoscopic surgeries, 10 were robotic surgeries, and 4 were open surgeries. |
Remarkable advances have been made in the treatment of stomach cancer.
Surgery has evolved from the previous open surgery with large incisions to minimally invasive surgery (laparoscopic surgery/robotic surgery) with small incisions and quick recovery, and the majority of surgeries performed in our department are minimally invasive surgeries (one endoscopic surgery technician certified (stomach area), and one robotic-assisted gastric surgery proctor).
Advances have been made in both surgical and medical treatments, and even patients with early-stage cancer who previously required surgery can now be cured with endoscopic resection. For this reason, even for patients referred to our department, we may recommend treatment at a gastroenterology department if necessary.
Furthermore, even for patients with advanced cancers for which surgery is not possible or for which a complete cure is difficult with surgery alone, an appropriate combination of anti-cancer drug treatment before and after surgery has made surgery possible or made the cancer completely curable. In recent years, anti-cancer drug treatment has become more complex as the number of options has increased, so we work closely with the oncology department, which specializes in this area, to appropriately manage side effects.
We will provide treatment that meets the patient's needs while making the most of the benefits of both surgical and medical treatments, so please feel free to consult us.
| 2023 | 131 cases (laparoscopic surgery: 77 cases, robotic surgery: 46 cases, open surgery: 8 cases) |
|---|---|
| 2022 | 110 cases (laparoscopic surgery: 70 cases, robotic surgery: 26 cases, open surgery: 14 cases) |
| 2021 | 95 cases (laparoscopic surgery: 65 cases, robotic surgery: 18 cases, open surgery: 12 cases) |
Our department actively performs laparoscopic surgery and robotic surgery (minimally invasive surgery) for colorectal cancer. Minimally invasive surgery is characterized by the fact that it can be performed by simply making multiple small incisions of 5mm to 1cm in the abdomen, which minimizes the burden on the patient. We also have three endoscopic surgery technicians (colon area) certified by the Japanese Society of Endoscopic Surgery, and one robotic rectal and colon surgery proctor, so we can perform safe and reliable surgeries.
In addition, by providing multidisciplinary treatments such as preoperative chemoradiotherapy and chemotherapy, we aim for a definitive cure and are able to provide surgical procedures that avoid the need for a colostomy whenever possible.We cooperate with the medical oncology department and the radiation therapy department as necessary to provide the most appropriate treatment for patients.
The average length of hospital stay after surgery is around 10 days, and we aim for patients to return to their daily lives and work as quickly as possible. In order to prevent recurrence as much as possible, we also provide postoperative adjuvant chemotherapy as needed. We have a system in place that allows us to provide a variety of treatments according to the patient's wishes, so please feel free to consult us.
| Indications for liver resection | Number of laparoscopic/open liver resections | |
|---|---|---|
| 2023 | 22 cases of primary liver tumors, 15 cases of metastatic liver tumors, 8 cases of other diseases (including biliary tract cancer) | 45 cases (29 laparoscopy, 16 laparotomy (including biliary tract cancer)) |
| 2022 | 24 cases of primary liver tumors, 12 cases of metastatic liver tumors, and 9 cases of other diseases (including biliary tract cancer). | 45 cases (23 laparoscopy, 22 laparotomy (including biliary tract cancer)) |
| 2021 | 17 cases of primary liver tumors, 14 cases of metastatic liver tumors, 15 cases of other diseases (including biliary tract cancer) | 46 cases (17 laparoscopy, 29 laparotomy (including biliary tract cancer)) |
At our hospital, liver surgeries are performed by a team of five staff members who specialize in hepato-biliary-pancreatic surgery (including two highly skilled hepato-biliary-pancreatic surgeons and specialists).
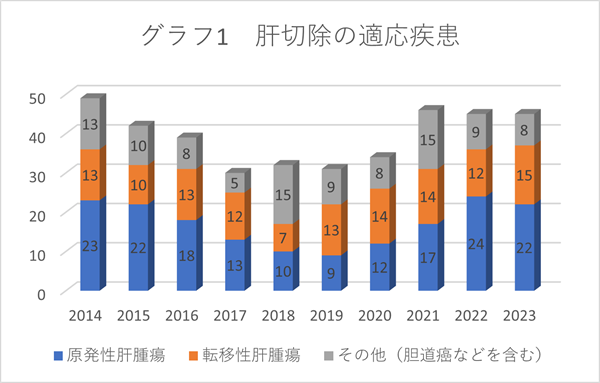
The diseases targeted are primary liver cancer (hepatocellular carcinoma, intrahepatic cholangiocarcinoma, etc.), metastatic liver cancer (metastasis of cancer from other organs to the liver, especially metastasis of colorectal cancer to the liver), and biliary tract cancer (bile duct cancer and gallbladder cancer) (see Graph 1).
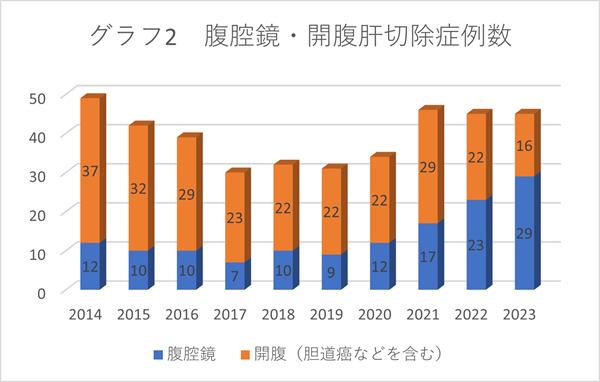
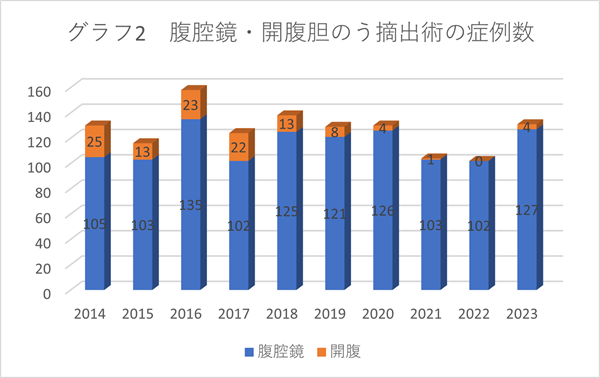
The proportion of minimally invasive surgery (laparoscopic surgery) is increasing year by year, and currently most cases are performed using minimally invasive surgery (see Graph 2). Open surgery is performed for biliary tract cancer, some primary liver cancers, and metastatic liver cancers (when there are many tumors or when there has been a history of multiple surgeries), and the surgical procedure is decided taking into consideration the difficulty of the surgery and the patient's wishes.
Treatment plans are decided after discussions at weekly conferences with gastroenterologists and radiologists. If there are multiple treatment options, we will decide on a plan after listening to the patient's wishes, so please rest assured.
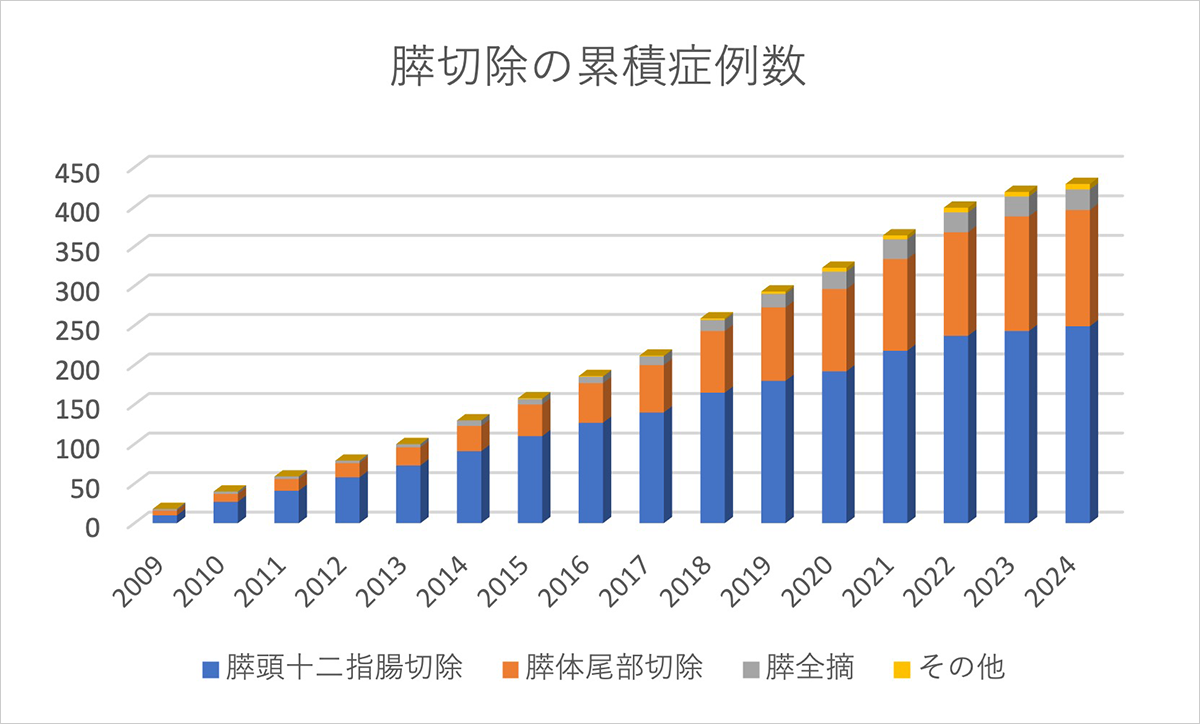
All pancreatic resection cases at our hospital (including surgeries for diseases other than pancreatic cancer):
From January 2009 to June 2024, there were 429 cases (average of approximately 28 cases per year)
(Pancreaticoduodenectomy: 249 cases, distal pancreatectomy: 147 cases, total pancreatectomy: 26 cases, other: 7 cases)
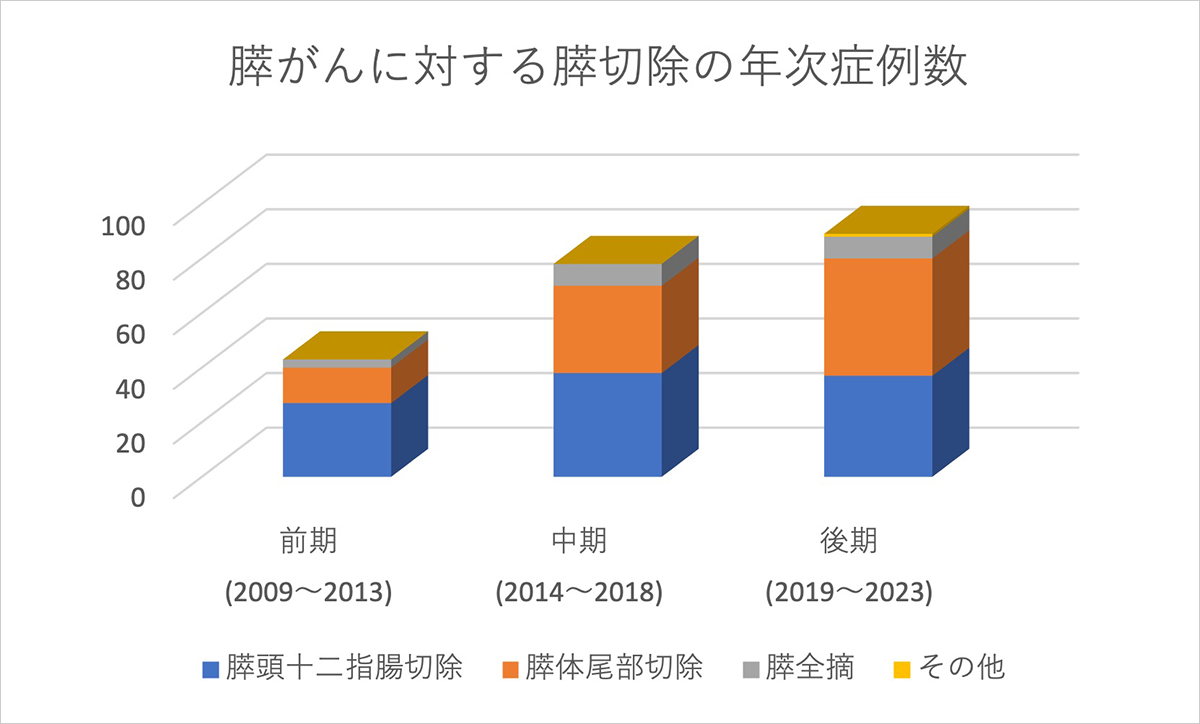
Of these, the number of surgical cases for conventional pancreatic cancer (excluding IPMN-derived pancreatic cancer) has been increasing since 2014.
| First half (2009-2013) | 43 cases (pancreaticoduodenectomy: 27 cases, distal pancreatectomy: 13 cases, total pancreatectomy: 3 cases) |
|---|---|
| Mid-term (2014-2018) | 78 cases (pancreaticoduodenectomy: 38 cases, distal pancreatectomy: 32 cases, total pancreatectomy: 8 cases) |
| Second term (2019-2023) | 89 cases (pancreaticoduodenectomy: 37 cases, distal pancreatectomy: 43 cases, total pancreatectomy: 8 cases, other: 1 case) |
Our hospital has been performing laparoscopic surgery for distal pancreatectomy for pancreatic cancer since 2018, and since 2019, we have performed this minimally invasive surgery in 27 cases (75%), which is approximately three-quarters of all cases.
The main treatment for pancreatic cancer is surgical resection, and based on imaging findings, it is classified into three types: 1) resectable pancreatic cancer, 2) borderline resectable pancreatic cancer, and 3) unresectable pancreatic cancer (locally advanced or with distant metastasis).
However, for pancreatic cancer, which is inherently highly malignant and has a high rate of postoperative recurrence, the therapeutic effect of resection alone is insufficient, so we aim to improve treatment outcomes through multidisciplinary treatment that combines preoperative treatment (chemotherapy and chemoradiotherapy) with postoperative adjuvant chemotherapy.
At our hospital, the gastroenterology department and the gastroenterology surgery department work closely together to share information from the initial consultation. If a diagnosis of pancreatic cancer is made, a treatment plan is created to start treatment as soon as possible (within one month at the latest).
Except for cases of clearly unresectable pancreatic cancer, exploratory laparoscopic surgery (approximately 1 hour) is performed on all resectable and borderline resectable pancreatic cancer patients to check for peritoneal dissemination and micrometastasis to the liver. The initial preoperative treatment is then administered during the patient's hospitalization.
After a period of preoperative treatment depending on the possibility of resection, surgical resection is performed. Note that laparoscopic surgery is the first choice for distal pancreatectomy.
After surgery, patients undergo six months of adjuvant chemotherapy (typically an oral medication called TS-1).
Another feature of our hospital is that we provide nutritional therapy support from a registered dietitian from an early stage in this multidisciplinary treatment period.
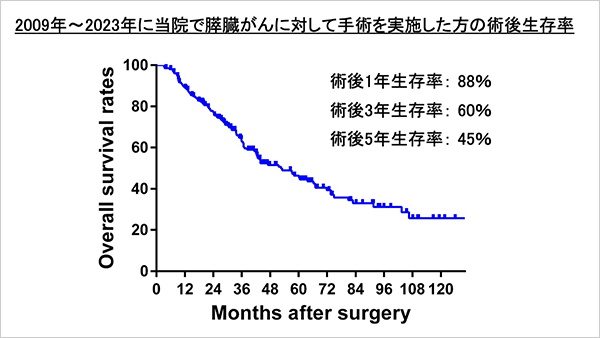
Finally, we will show the treatment outcomes of pancreatic cancer surgeries (206 cases) performed between 2009 and 2023.
3-year survival rate: 63.51 TP3T, 5-year survival rate: 46.41 TP3T, median survival time: 52.5 months
Cases of recurrence-free survival for 5 years or more: 29 cases (as of July 10, 2024)
Our hospital is well-equipped to provide the latest treatments tailored to each patient's condition, so please feel free to consult us at any time.
| Indications | Laparoscopy/laparotomy number | |
|---|---|---|
| 2023 | 97 cases of gallstones/cholecystitis, 26 cases of polyps/adenomyoma, 8 other cases | 127 laparoscopic cases, 4 open cases |
| 2022 | 81 cases of gallstones/cholecystitis, 15 cases of polyps/adenomyoma, 6 other cases | Laparoscopy: 102 cases, laparotomy: 0 cases |
| 2021 | 89 cases of gallstones/cholecystitis, 13 cases of polyps/adenomyoma, 2 other cases | Laparoscopy 103 cases, laparotomy 1 case |
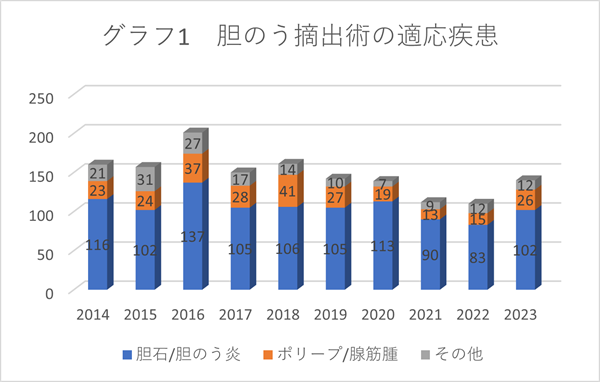
Diseases that may require cholecystectomy include gallstones, cholecystitis, gallbladder polyps, adenomyomatosis of the gallbladder, and gallbladder cancer (or suspected cancer) (see Graph 1).
Gallstones are formed when components of bile stored in the gallbladder solidify. Many people with gallstones are asymptomatic, but some may experience pain due to gallstone attacks or cholecystitis, and surgery is recommended for such people.
Gallbladder polyps and adenomyomatosis are asymptomatic in most cases, but it is often difficult to distinguish them from gallbladder cancer, and in such cases surgery is recommended.
In either case, surgery involves removing the gallbladder. Our department performs approximately 100 to 150 cholecystectomies each year, and currently, as a rule, we perform these procedures using minimally invasive surgery (laparoscopic surgery) (see Graph 2). In cases of severe cholecystitis, we may perform open surgery, or switch to open surgery midway through the procedure.
| 2023 | 115 cases (76 cases of laparoscopic surgery, 39 cases of anterior open surgery) |
|---|---|
| 2022 | 82 cases (61 cases of laparoscopic surgery, 21 cases of anterior open surgery) |
| 2021 | 91 cases (61 cases of laparoscopic surgery, 30 cases of anterior open surgery) |
A hernia is a condition in which the abdominal muscles become loose and the intestines or other organs protrude, requiring surgical treatment. Most hernias occur in the groin area (the base of the thighs), but abdominal wall hernias that occur around the navel or after abdominal surgery can also be treated.
Our department actively performs laparoscopic surgery under general anesthesia, which leaves small scars and places less strain on the patient. However, for those whose conditions make general anesthesia or laparoscopic surgery unsuitable, we provide appropriate surgical treatment, taking into consideration the condition and wishes of each individual patient, such as anterior incision surgery.
The length of hospital stay after surgery is approximately two days. We support patients to achieve a return to society as soon as possible, and many patients have actually returned to work immediately after being discharged from the hospital. If you are concerned about swelling in the groin or abdomen, please feel free to contact us.
| 2023 | 134 cases (acute appendicitis 63 cases, acute cholecystitis 24 cases, intestinal obstruction 15 cases, gastrointestinal perforation 14 cases, incarcerated hernia 8 cases, other 10 cases) |
|---|---|
| 2022 | 137 cases (58 cases of acute appendicitis, 29 cases of acute cholecystitis, 19 cases of intestinal obstruction, 14 cases of gastrointestinal perforation, 11 cases of incarcerated hernia, and 6 other cases) |
| 2021 | 153 cases (acute appendicitis 63 cases, acute cholecystitis 36 cases, intestinal obstruction 16 cases, gastrointestinal perforation 21 cases, incarcerated hernia 6 cases, other 11 cases) |
Our department actively provides medical care for abdominal emergencies, including acute appendicitis and acute cholecystitis. After properly assessing the necessity of surgery, we provide surgical treatment if necessary.
Surgery for abdominal emergencies is not limited to open surgery; depending on the disease, minimally invasive surgery is often possible, and we actively adopt laparoscopic surgery, which involves making multiple small holes measuring 5 mm to 1 cm in the abdomen.
After surgery, depending on the severity of the condition, we work with the intensive care unit to continue medical care through hospitalization and outpatient care, striving to allow patients to live their daily lives with peace of mind. Abdominal emergencies vary in severity depending on the disease. We will provide appropriate treatment, including surgery, depending on the patient's condition, so please feel free to consult us.